NIH establishes UC Davis-LLNL Center for Point-Of-Care Technologies to speed detection of bloodstream infections
Doctors one day may be able to diagnose bloodstream infections within one hour rather than waiting a day to several days for conventional test results from labs.
And, instead of transporting a blood sample to a hospital, doctors may well have the capability to render a diagnosis at an emergency shelter or at the scene of a disaster.
These and other advances are expected to result from a five-year, $8.5 million grant awarded recently to doctors, scientists and engineers who are part of a team from UC Davis Health System and Lawrence Livermore National Laboratory (LLNL) that will focus on point-of-care testing (POCT). POCT is defined as diagnostic testing at or near the site of patient care.
The grant, from the National Institute of Biomedical Imaging and Bioengineering (NIBIB), part of the National Institutes of Health, will fund the development of two prototype instruments that simultaneously detect five bacterial and fungal pathogens. The grant also funds evaluations of other exploratory diagnostic technologies intended to prepare the nation for future disasters.
The work will be undertaken through the UC Davis-LLNL Center for POC Technologies, which is part of the newly established NIBIB POC Technologies Research Network.
"The goal of our center is to improve the accessibility, portability and field robustness of POC instruments for critical-emergency-disaster care in community hospitals, rural areas and disaster response sites," said Gerald Kost, professor of Pathology and Laboratory Medicine and director of the POCT•CTR at UC Davis Health System.
Events during Hurricane Katrina demonstrated the basic feasibility of POCT, but follow-up laboratory experiments showed that current equipment is not adequate for field use, said Kost, the grant’s principal investigator.
"We need rapid diagnostics and rugged instruments for use in disasters," Kost said. "Rescues were slowed during Katrina because hospitals were out of commission. Doctors didn’t have adequate tools needed to make fast diagnoses; treatment was delayed. Instruments could not stand the environmental stresses."
"Research is needed to develop field-worthy, battery-operated devices robust enough to withstand extreme ranges of humidity, temperature and altitude encountered during rescue operations," Kost said. "Reagents, test strips and quality-control materials must withstand the same harsh conditions, because it is difficult or impractical to transport materials in environmentally controlled containers that are either refrigerated or heated."
The diagnostic instruments to be developed will be easy to use with minimal training and rugged, so they can be deployed in challenging environments, said LLNL chemist Ben Hindson, who with chemical engineer John Dzenitis, is directing the grant work at the Laboratory.
"We see these technologies as assisting medical personnel to be able to make fast and accurate disease diagnoses, so they can administer the proper medicine and save lives during natural disasters," Hindson explained.
Under the grant, the LLNL-UC Davis research team will develop two prototype detection instruments – one for hospital settings and one that is field portable.
UC Davis researchers will assist with the instrument design, evaluate and clinically test prototypes, solicit input from users on what works and what doesn’t work, educate health care teams, and train rescue workers to use the devices, among other tasks.
The LLNL Pathogen Informatics Group, with assistance from UC Davis researchers, will use its capabilities to design unique DNA signatures or assays for use with the new instruments. The five pathogens for which unique identification signatures will be developed under the grant are:
- Methicillin-resistant S taphylococcus aureus (MRSA) is a bacterium associated with catheter-related line infections, and skin and soft tissue infections. MRSA also appears in community settings, such as schools.
- Pseudomonas aeruginosa is a bacterium often linked to hospital-acquired bloodstream infections and associated with pulmonary complications, such as respiratory distress syndrome. People whose wounds have been contaminated with fresh water or water-soil mixtures are more likely to contract infections from this bacterium.
- Escherichia coli is one of the more common organisms found among patients who contract hospital-acquired infections. This pathogen also is the most frequent community-acquired bacterium in urinary tract infections and occasionally shows up in food products, such as contaminated ground beef and salad greens.
- Streptococcus pneumoniae is the most common cause of severe community-acquired pneumonia. A survey of UC Davis Medical Center intensive care staff found that this bacterium was one of the key pathogens identified by clinicians, who said more rapid detection could help ensure early appropriate antimicrobial treatment.
- Candida yeast infections affect people with weakened immune systems, such as transplant recipients on immunosuppressants, cancer patients receiving chemotherapy or patients with acquired immune deficiency syndrome (AIDS).
"These five pathogens were selected based on their clinical significance, occurrence in hospitalized patients, threat to the community, and frequency of being isolated from the wounds of victims of severe weather- and flood-related natural disasters," Kost said.
Infections with any one of the five pathogens can lead to the complex disease syndrome of sepsis, a systemic response leading to widespread and uncontrolled activation of inflammation and coagulation pathways. Sepsis represents one of the primary causes of death in hospitalized patients worldwide.
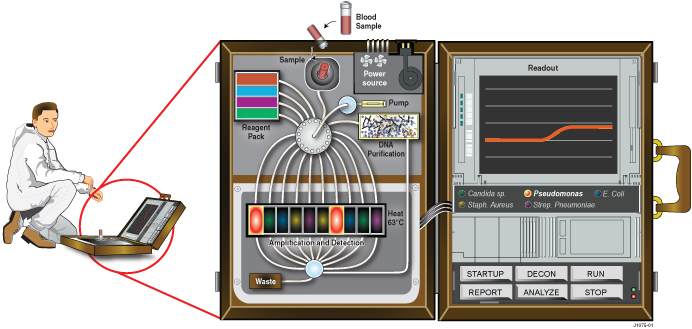
As envisioned, blood samples would be loaded into the LLNL-UC Davis instruments, which would automatically handle all of the processing steps.
Instead of relying on the polymerase chain reaction (PCR) technique, the instruments will use a new DNA amplification method called loop mediated amplification (LAMP).
The LAMP method uses a portion of the Bacillus stearothermophilus DNA polymerase protein, an enzyme that splits the double strand of DNA and allows it to be copied at a single temperature (63 degrees Celsius or 145 degrees Fahrenheit), rather than using multiple cycles of heating and cooling, as PCR requires.
Initially, using a blood sample from one person, the instruments will run a simultaneous test for all five pathogens within one hour. Eventually, the team hopes to outfit the instruments with the capability to run tests for all five pathogens within an hour for several people at the same time, Hindson said.
Several LLNL-developed biodetection technologies, such as the Autonomous Pathogen Detection System, that are designed to protect against bioterrorism, will provide some of the foundational technologies for these new POC instruments.
One strength of the UC Davis-Livermore team is its ability to leverage the "bench to bedside" skills of the UC Davis Clinical and Translational Science Center (CTSC) headed by Lars Berglund. The CTSC was established at UC Davis in 2006 by the National Institutes of Health as one of the NIH’s 12 initial national centers for improving the yield of medical research.
The grant also draws on the infrastructure provided by the UC Davis-LLNL Center for Biophotonics Science and Technology (CBST), which is headed by Dennis Matthews of both UC Davis and LLNL. CBST was funded by the National Science Foundation in 2002 and creates optical technologies for medicine and bioscience.
In addition to the UC Davis-LLNL Center for POC Technologies, the NIBIB has established three other centers for cooperative research: emerging neurotechnologies, at the University of Cincinnati; sexually transmitted diseases, at Johns Hopkins University; and diagnostics for global health, at PATH Seattle and the University of Washington.
UC Davis Health System is the leading tertiary care provider for a 33-county region of Northern California. Research strengths at UC Davis Health System include clinical and translational science, stem cell science, infectious diseases, vascular biology, neuroscience, cancer, functional genomics and mouse biology, comparative medicine, combinatorial chemistry and nutrition, among many others.
Founded in 1952, Lawrence Livermore National Laboratory has a mission to ensure national security and to apply science and technology to the important issues of our time. Lawrence Livermore National Laboratory is managed by Lawrence Livermore National Security, LLC for the U.S. Department of Energy's National Nuclear Security Administration.