Lab and UC Davis know-how find new ways to fight cancer
Eight years ago, when the UC Davis Cancer Center and the Laboratory agreed to collaborate on an integrated cancer program, hopes were high. The Laboratory had spent nearly 50 years developing military technology to ensure the country’s security, while the Cancer Center was becoming an integral part of the war on cancer. The partnership was the first of its kind.
Little did organizers know just how many advances would quickly flow from this unique combination of resources and talent:
- Design of a compact proton beam accelerator that could make the benefits of proton radiation therapy widely available to cancer patients, with the first conceptual prototype expected by the end of this year.
- Research into technologies that hold promise for dramatic improvements in diagnosis and treatment of such illnesses as non-Hodgkin's lymphoma and prostate, breast and bladder cancers.
- National Cancer Institute designation for the Cancer Center in 2002, transforming the center into the only NCI-designated center between San Francisco and Portland, with the LLNL research partnership playing a key role in winning the honor.
- The establishment in 2002 of the Center for Biophotonics Science & Technology at UC Davis, serving as an incubator for biomedical applications of laser and related biophotonics instrumentation, starting with LLNL talent and technologies.
"It’s been a perfect fit," says longtime Laboratory senior bioscientist Jim Felton, who helped craft the alliance and is now associate director of cancer control at the Cancer Center.
"Lawrence Livermore scientists were in need of human disease experts and patients to advance their studies, and UC Davis saw the advantage of working with national lab technologies. Now, eight years later, we’re seeing the blossoming of this exciting collaboration."
In many ways, it’s been a one-of-a-kind collaboration that can serve as a model for other programs, universities and national laboratories. The partnership has led to similar collaborations with other units at UC Davis, including a new pandemic medicine center where Laboratory technology innovations are central, and new research to study traumatic brain injury and related neurological disorders.
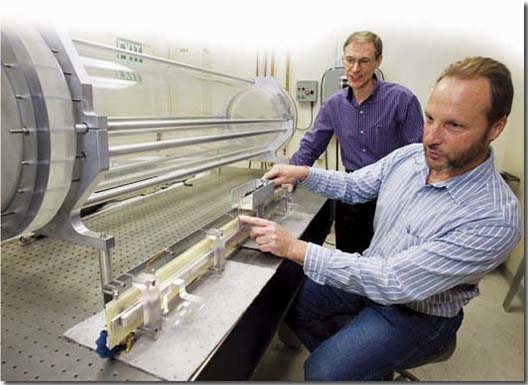
Proton-beam accelerator
Of the myriad research projects that have come out of the alliance, the compact proton-beam accelerator is one of the most promising in the development pipeline. It holds tantalizing potential for changing the radiation therapy landscape.
Proton-beam therapy involves the use of cyclotrons or synchrotons — which accelerate charged particles using a high-frequency, alternating voltage — to irradiate cancerous tissue. Evidence shows that it’s as effective as other radiation therapies, but with fewer side effects. In prostate cancer, for instance, post-radiation incontinence or impotence are often reported to be lower with proton-beam therapy.
However, large size and high cost — necessitated in part by the use of a huge bending magnet within the device — have prevented wide implementation. Installation can cost up to $200 million and can require square footage the size of a typical hospital building.
Soon after he became director of the Center for Biophotonics Science & Technology in 2002, Dennis Matthews, who also serves as the Cancer Center’s associate director for biomedical technology, hit upon a potential solution.
He was aware of efforts led by Lab physicist George Caporaso to develop a compact proton-beam accelerator for military applications, one that sidestepped the need for that large magnet by using what is known as dielectric wall accelerator technology. He suggested adapting that design to cancer treatment applications.
His winning idea took hold, and today, Caporaso and his team are on their way to delivering a subscale prototype by December. The technology, licensed last year to Madison, Wis.-based TomoTherapy, holds promise to dramatically lower costs associated with proton-beam therapy and thus to make it widely available for the benefit of cancer patients everywhere.
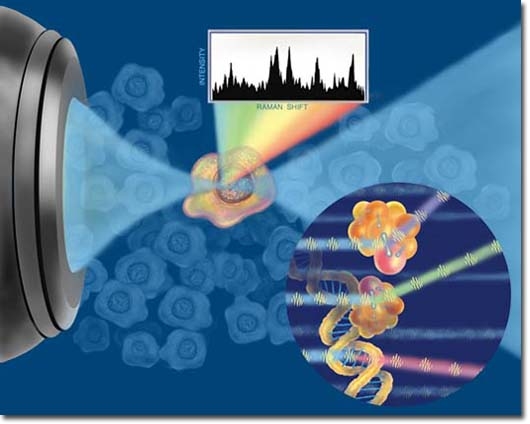
Laser tweezer Raman spectroscopy
Researchers at the biophotonics center and at the Lab are refining a combination of two technologies for cancer diagnosis, with an initial emphasis on leukemia cells. Called laser tweezer Raman spectroscopy, the breakthrough technique could lead to quick identification of cancer cells through analysis of the nuclei of individual cells, all done without damaging the tissue sample, unlike current methods.
This subcellular technique marries Raman spectroscopy, a method of analyzing samples using laser light, and the more recently developed use of laser beams to hold floating cells in place. The current average analysis time is one to two minutes per cell. The ambitious goal of the research is to greatly improve that speed and efficiency, and from there to commercialize the technology so that it can be used widely.
"This is a completely new technology with much more potential than any technique that’s been used until now," says UC Davis pediatric oncologist Douglas Taylor, who is developing the technology with Thomas Huser, chief scientist at the biophotonics center, and LLNL staff scientist James Chan.
Ligands, accelerator mass spectrometer and more
Rod Balhorn, a Laboratory biochemist and group leader for molecular toxicology, is working with UC Davis researchers Gerald and Sally DeNardo on a refinement of radioimmune therapy, a well-established method for treating cancer patients with antibodies that carry radioactive metals. In this therapy, the antibody molecules attach themselves to tumors by binding to proteins on the outside of cancer cells, bringing the radioactivity close to the cell to deliver local radiation.
Balhorn and his research team are creating small molecules called SHALs that mimic the binding of antibodies to tumor cells. This is accomplished by connecting two ligands that bind to neighboring sites on a protein found on tumor cells. That connectivity greatly increases the molecules’ effectiveness and strength of binding. The therapeutic value of this technique looks promising in early animal model studies.
Collaborations also involve use of the Lab's biomedical accelerator mass spectrometer, exceptional in its ability to sensitively and accurately analyze samples, for such applications as:
- Determining the human cancer risk posed by carcinogens in cooked meats, particularly the increased risk of prostate cancer from a particular carcinogenic compound called PhIP; and
- Microdosing, a technique for studying the behavior of compounds inside a body through the administration of doses so low that they are unlikely to produce whole-body effects, yet high enough to allow the cellular response to be studied.
Kris Kulp of the Laboratory's Bioanalytical Group is working with cancer center colleagues to develop a type of imaging mass spectrometry called ToF-SIMS, short for time-of-flight secondary ion mass spectrometry, to image and analyze different types of cancerous tissue. The ultimate goal is to provide more accurate predictions of which tumors are likely to grow aggressively (and thus require early attention) versus slow-growing tumors.
Laboratory staff scientist Stavros Demos, who also is a UC Davis associate adjunct professor, has joined with UC Davis researchers to develop optical biopsy instrumentation for real-time cancer detection, with an emphasis on bladder cancer.
A related project involves detection of cancer of the esophagus. Among the many benefits are on-the-spot pathological diagnoses, the enhancement of current endoscopes and the ability to target any later biopsies to regions most likely to contain cancerous cells.
Unique opportunities
These are just the highlights among a great many collaborative initiatives, Matthews says.
"The cancer center fosters discussion of the needs in cancer research, and by stirring Lawrence Livermore staff members into the mix — people who are first-rate physicists, engineers, chemists, biochemists, cell biologists and biologists — together they can identify and solve cancer problems," he said.
UC Davis Cancer Center Director Ralph deVere White, who, like Felton and Matthews, helped seal the original collaboration, agrees.
"Our integrated program has offered unique opportunities to scientists at Lawrence Livermore and to physicians and basic scientists at UC Davis," deVere White said.
"It has demonstrated the collateral benefit of using technology that was originally created to defend the country for quite a different purpose: to defend us all against the ravages of cancer."
© UC Regents 2008 UC Davis Medicine, Summer 2008 Reprinted with permission