Lab researchers and collaborators to develop new vaccine against three biothreat pathogens
 (Download Image)
(Download Image)
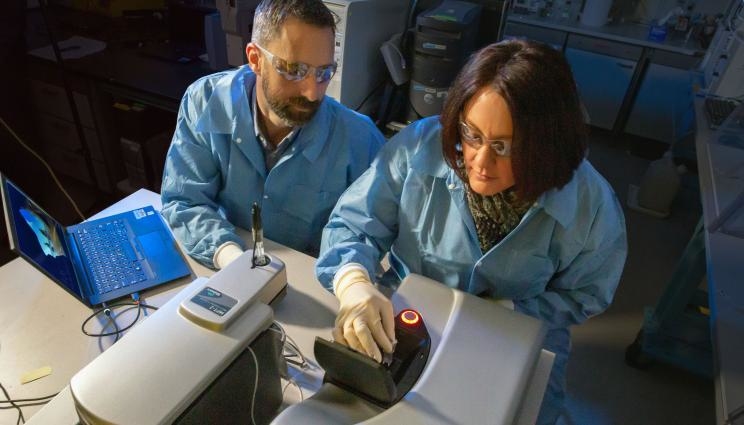
LLNL researchers Nick Fischer and Amy Rasley are characterizing nanolipoprotein particle vaccine formulations using a dynamic light-scattering instrument. Detailed characterization of the nanoparticles provides an important quality control metric for vaccine development. Photo by Julie Russell/LLNL.
Scientists from Lawrence Livermore National Laboratory (LLNL) and three other institutions are seeking to develop a multi-pathogen vaccine that will protect against three bacterial biothreat pathogens.
Led by LLNL, the team includes disease experts from the University of New Mexico Health Sciences Center (UNMHSC), the University of Nevada, Reno School of Medicine (UNR Med) and the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID).
The researchers, who will collaborate under a five-year, $10 million grant from the Defense Threat Reduction Agency (DTRA), are aiming to develop a single vaccine that will protect against tularemia, melioidosis and plague.
LLNL scientists have demonstrated the ability of a subunit vaccine, incorporating different antigens from the Francisella tularensis bacterium into a single particle, to protect against inhalation of high doses of this bacteria. F. tularensis is the bacteria that causes the disease tularemia, also known as rabbit fever.
Their collaborators at UNR Med and USAMRIID have been testing candidate subunit vaccines for melioidosis and plague respectively, and their data suggests that those subunit vaccines could be effective.
Kris Kulp, leader of the Lab’s Biosciences and Biotechnology Division, noted that the three-way vaccine, if successful, will protect against several high-priority pathogens in a single dose, greatly facilitating the defense of U.S. troops against biothreats.
“Not only will a simplified immunization regime be cost-effective, it also will enable warfighters to be fully vaccinated more quickly. This project builds on LLNL expertise using nanoparticle technology to deliver vaccines against single pathogens and takes them to the next step by adding antigens that will protect against multiple pathogens simultaneously,” Kulp said.
LLNL biologist Amy Rasley, who is co-principal investigator on the project with fellow Lab biologist Nick Fischer, calls the concept of a multi-pathogen vaccine that can protect against several biothreat pathogens at once “game-changing.”
“The development of such a vaccine presents exciting technical challenges associated with understanding the interactions of the vaccine components with each other and with our immune system, as well as in the manufacturing and testing of such vaccine formulations. We are thrilled to be part of this first step in looking at the feasibility of such an approach,” Rasley added.
Fischer noted, “We are gratified that our nanotechnology platform is being widely tested and applied to a wider range of difficult-to-treat pathogens and diseases. This effort mirrors the F. tularensis vaccine development we started in 2019.”
In addition to the four institutions, a Bay Area vaccine company — San Carlos-based Vaxcyte, Inc. — will produce Yersina pestis and F. tularensis antigens in a manner that is scalable and amenable to production in a “good manufacturing practices” environment.
The team’s scientists will build on a nanotechnology — called nanolipoprotein particles (NLPs) — that was developed at LLNL for delivering vaccines and drugs inside the human body.
NLPs are water-soluble molecules that are 6 to 30 billionths of a meter in size and resemble HDL particles, which are associated with playing a role in regulating the human body’s good cholesterol. LLNL scientists have worked on this nanotechnology, also known as nanodisc, since 2005.
Using the NLPs as a delivery platform, the antigens for the three disease-causing bacteria could be co-delivered with an adjuvant molecule, which stimulates the immune response against the antigens.
Terry Wu, a tularemia expert at UNMHSC, said, “We are excited to expand our collaboration with LLNL to develop subunit vaccines important for national defense and public health.”
Wu and his UNMHSC team will provide expertise to evaluate the safety and efficacy of the multi-pathogen vaccine against pneumonic tularemia.
At Fort Detrick, Md.-based USAMRIID, Joel Bozue and Christopher Cote will provide immunological characterizations of novel vaccines and perform efficacy studies using a mouse model of pneumonic plague.
Additional USAMRIID studies will test the LLNL tularemia vaccine to determine if it is able to protect rats in a pneumonic tularemia model against a diverse panel of F. tularensis strains from clinical and environmental samples.
UNR Med researchers Paul Brett and Mary Burtnick, who have more than 50 years combined experience studying the pathogenic Burkholderia species, will provide their expertise on Burkholderia pseudomallei for the multi-pathogen vaccine.
F. tularensis is classified as a class A high-priority pathogen and Tier 1 select agent by the Centers for Disease Control and Prevention (CDC). It is considered a potential biothreat agent based on its extremely low infectious dose. Disease manifestations vary depending on the route of exposure. It is an infectious disease that can cause fever, skin ulcers, enlarged lymph nodes, pneumonia and throat infection with inhalational disease (pulmonary tularemia) being most severe.
Plague is an infectious disease responsible for killing millions during the Middle Ages and is caused by the bacterium Yersinia pestis. While antibiotic treatment is effective against plague, the disease is associated with high mortality rates when contracted via inhalation (pneumonic plague). Due to its extreme virulence, ability to be aerosolized and previous historical use as a bioweapon, it is classified as a Tier 1 select agent by the CDC. Plague continues to be endemic worldwide.
Melioidosis is an infectious disease, predominant in tropical climates, caused by the bacterium B. pseudomallei. Melioidosis is typically contracted through inhalation of contaminated dust or water droplets or through contact with contaminated soil. Antibiotic treatment for melioidosis is prolonged, often three to eight months, and the disease is associated with high mortality rates when contracted via inhalation. The CDC classifies B. pseudomallei as a Tier 1 select agent.
In 2019, LLNL and two other institutions (UNMHSC and the Tulane National Primate Research Center) received a five-year, $7.5 million grant from DTRA to accelerate the testing of an NLP-based tularemia vaccine.
In addition to Fischer and Rasley, other LLNL biomedical scientists who are part of the team working to develop the multi-pathogen vaccine are Sean Gilmore, Sandra Peters and Dina Weilhammer.
Contact
 Stephen Wampler
Stephen Wampler
[email protected]
(925) 423-3107
Related Links
"A Long Shot Pays Off In Vaccine Development"Defense Threat Reduction Agency
University of New Mexico Health Sciences Center
University of Nevada, Reno School of Medicine
U.S. Army Medical Research Institute of Infectious Diseases
LLNL Innovation and Partnerships Office
Tags
Bioscience and BioengineeringBiosciences and Biotechnology
Global Security
Physical and Life Sciences
Science
Threat preparedness
Counterterrorism
Featured Articles







