Journal highlights Lab testing of 3D-printed COVID-19 nasal swabs
 (Download Image)
(Download Image)
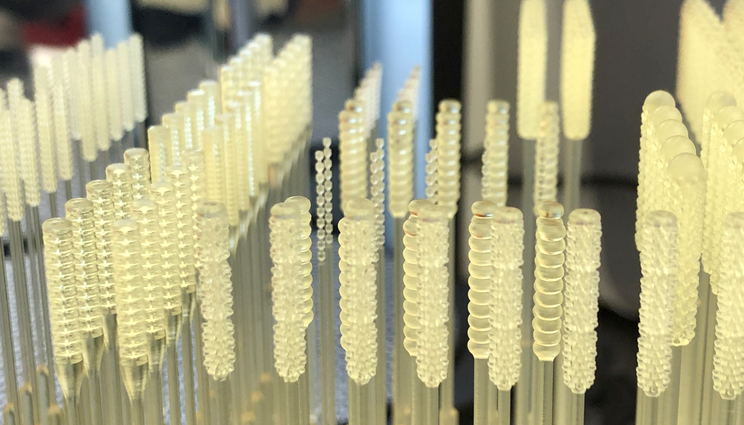
Given the early supply chain issues associated with the delivery of COVID-19 testing and prevention efforts, scientists and engineers at Lawrence Livermore National Laboratory focused efforts on novel modes of production for existing consumables, including 3D-printed nasopharyngeal testing swabs. The work was highlighted in a recent issue of the Materials Research Society Bulletin. Photo by Angela Tooker/LLNL.
Lawrence Livermore National Laboratory’s work on consumables for COVID-19 testing was highlighted in a recent special issue of the Materials Research Society (MRS) Bulletin focusing on materials science innovation in response to the pandemic.
Guest-edited with an introduction by Crystal Chu (Lehigh University), Claire Witherel (University of Pennsylvania) and LLNL research scientist Salmaan Baxamusa, the issue also includes an article from a Lab team led by Microfabrication Research and Development Engineer Angela Tooker on testing COVID-19 nasopharyngeal swabs.
The issue’s introduction offers a brief overview of consumables produced in the context of COVID-19 and the need for rapid iteration and testing of medical technologies. Some of the need was caused by manufacturing and supply-chain challenges, and some was a need for more accessible or more rapid diagnostics than the PCR tests that have become the go-to for reliable COVID testing. All require the expertise of materials scientists.
Given the early supply-chain issues associated with the delivery of COVID testing and prevention efforts, scientists and engineers focused efforts on novel modes of production for existing consumables. At LLNL, the production of nasopharyngeal testing swabs was among the endeavors undertaken to address such shortages.
Materials science and manufacturing innovation in the production of nasopharyngeal swabs resulted in the need for a quantitative assessment of their performance as well as robust testing protocols for general use. Led by Tooker and Materials Engineering Division Leader Chris Spadaccini, the protocol developed at LLNL aimed to provide a reliable, quantitative set of methods for understanding the aspects of swabs that are crucial to reliable COVID testing: collecting enough of a sample for RNA to be extracted from it; and producing structural soundness that doesn’t come at the expense of flexibility and patient comfort.
With traditional nylon-flocked swabs as the point of reference, Tooker and her team, among others in the scientific community, sought to 3D-print nasopharyngeal swabs that would perform similarly but would offer an alternate production method to make up for shortages in the production of flocked swabs. 3D printing offers both an accelerated prototyping timeline and a wider diversity of manufacturing materials, so their primary advantages early in the pandemic were to create a new supply chain and allow for on-demand, point-of-care manufacturing. As the authors suggest: “3D printers already in use in hospitals and clinics could easily be repurposed, allowing those entities to 3D-print their own swabs to meet demand.”
To develop a universal testing protocol, Tooker and the team conducted tests of six swab types that hadn’t all been subjected to testing that accounted for typical usage scenarios. They tested the following aspects of both flocked swabs and a range of 3D-printed swabs: sample collection and usability (after a normal time lapse), abrasion and mechanical performance (tensile strength, torsion, flexibility and breakpoints).
Sample collection requires that the swab collect both mucus and cells from the nasopharynx, retain them and release them. To test these abilities, swabs collected samples from infected “mucus mimic” and cells, which were then incubated in a medium for 2.5 to 4 hours.
Despite 3D-printed swabs’ lack of absorbency compared to flocked swabs, prototypes whose swab heads had lattice structures were able to collect sufficient mucus and cells while preserving patient comfort to perform comparably or better than traditional swabs. These prototypes can more easily be varied according to patient nostril size and made more comfortable for children, the authors concluded.
When it came to cycle threshold (CT) values, 3D-printed swabs performed on par with flocked swabs. CT indicates how many times a machine needs to copy the virus’s RNA so that it can be detected on a PCR (polymerase chain reaction) test — a lower CT value typically indicates that more virus is present, because fewer cycles are needed to trigger a PCR result. The 3D-printed and flocked swabs took up similar amounts of virus and RNA for testing.
Most aspects of mechanical performance were evaluated on a standard tensile testing machine while torsion and combined torsion and flexure were evaluated using a rheometer. The machines were calibrated to mimic the bendability experienced when a swab is inserted into the nose, the torsion of the swab when rotated within the nostril and the tension caused when a swab is removed. This was done at multiple time intervals to account for any degradation associated with sterilization and shelf-aging during transport.
On tests of tensile strength and torque, 3D-printed swabs performed better than flocked swabs, the team found. However, they proved less flexible than flocked swabs, which may account for their increased abrasiveness. While none of the 3D-printed swabs broke despite reduced flexibility, the authors noted that they may be less tolerated by patients, since higher abrasion can translate to more nasal discomfort or even injury. Additionally, some 3D-printed swabs showed less tensile strength after being stored and sterilized, suggesting to researchers that autoclaving may make samples more susceptible to aging.
In addition to their increased strength, the testing protocol developed by Tooker and her colleagues showed that 3D printed swabs “were found to have fewer false positives compared to traditional swabs, further highlighting the need to improve sample collection for all types of swabs to improve diagnostic testing sensitivity,” according to the paper.
Among other papers on consumables at the intersection of biosensory and materials science, the special issue included articles describing novel biosensors that give new insight into host-pathogen interactions and another describing the biomaterials research that led to the development of the Pfizer and Moderna lipid nanoparticle-based mRNA vaccines.
Editors Baxamusa, Chu and Witherel point out that, in contexts other than the COVID-19 pandemic, nanoparticles have been instrumental in distributing medical antibodies and show promise for combating widespread threats to health in the future.
To learn more about COVID-19 response work done at national laboratories, read the article on COVID-related respirators and filtration media recently done at Oak Ridge National Laboratory, Lawrence Berkeley National Laboratory and Argonne National Laboratory.
-- Aimee Fountain
Contact
 Jeremy Thomas
Jeremy Thomas
[email protected]
(925) 422-5539
Related Links
Materials Research SocietyLab provides assistance in national swab shortage
LLNL COVID-19 Research and Response
Tags
EngineeringFeatured Articles